To The American Congress of Obstetricians and Gynecologists (ACOG):
As it relates to stillbirth and infant death, it’s time to wake up. Or, in other words, it’s time to get it together. Because it’s 2016 – the supposed age of information and communication and technology and the internet and fact checking and developments and breakthroughs and progressive ideas. And, in 2016, in the United States of America, there should be few, if any, excuses.
But, instead, the excuses run oh-so-sickeningly rampant. So any real progress remains stunted. Or non-existent, really – left to efforts of educated, aggressive patients, grass roots movements and small non-profit organizations, technology companies, and special lone-wolf-type medical professionals who possess the curiosity and energy necessary to attempt to initiate change. Because, certainly, you’ve made few such efforts.
Since losing my first born child in July of 2015, I continue to be blown away (in the worst way possible) every time I find myself involved in a conversation related to the medical side of stillbirth. I can’t believe the things I hear over and over and over again.
And said unbelievable things generally don’t come from fellow bereaved parents. They come from you – via your affiliated medical professionals, who do an exemplary job delivering your message, always crediting it to you.
I know because any time I challenge one of your affiliated medical professionals, he/she quickly throws up the white flag, often acknowledges I’m indeed correct, but then explains, “Stillbirth prevention isn’t a priority because of ACOG. Standard of care isn’t so great because of ACOG. Etc.”
So many things are “because of ACOG” that I’m confident my anger isn’t misdirected.
And I often feel like I’m stuck in the ‘60s when I’m confronted with you and your affiliated medical professionals’ attitude towards stillbirth. Because this information is generally so out-of-date, many times grossly inaccurate, and frequently debunked by a simple google search.
So then I wonder if you just think we’re all stupid. Or I wonder if you and your affiliated medical professionals are incompetent. But then I remind myself this probably isn’t the case either. Most likely, many of you are highly intelligent and competent, rather primarily concerned with minimizing legal liability, which I acknowledge, in our country, with our broken healthcare system, must be a challenge. (Believe me, I don’t envy you for having to weigh these considerations.)
Though none of these complexities change the fact that I’m still frequently left completely baffled upon hearing the things your affiliated medical professionals say – things so ridiculous they should never be spoken again. Things you should never want spoken again. Because they’re false. And they’re misleading. And to those who know better, they make you and your affiliated medical professionals look embarrassingly inept.
So, while I acknowledge this is a broad topic with a million and one complexities, I implore you, at the very least, to consider banning the below phrases from further use among your affiliated medical professionals, many of whom, I acknowledge, probably spew said phrases out of desperation, because you so often tie their hands as it relates to them actually being able to implement tangible changes within their practices (a topic for another day). But the below phrases should be banned regardless…
“This (stillbirth) just happens sometimes.”
Stillbirth doesn’t “just happen sometimes.” Maybe 50 years ago it did. But not anymore. At least not in all 26,000 instances per year.
There is a medical reason for most of these deaths. A reason you and your affiliated medical professionals should be curious about. A reason likely identifiable upon a full post-mortem investigation. A reason that, in thousands of cases, could’ve been identified before death occurred, allowing for potential management to a better outcome.
Patients with other ailments aren’t simply told, “This just happens sometimes.” And it should be no different with stillbirth, one of life’s most tragic events. At least not before you try harder. “This just happens sometimes” is never an acceptable first response, rather it should be the last response.
“This (stillbirth) is like being struck by lightning.”
You know what’s wrong with this analogy? It’s so inaccurate and misleading it borders on unethical. Because who’s actually scared of being struck by lightning? Answer – no one. Because it’s extremely rare – a 1/12,000 chance.
1/160 pregnancies end in stillbirth. Therefore, the lightning strike analogy simply doesn’t accurately convey the true likelihood of this possible outcome to those discerning patients who want to know – who base their level of worry, and possibly their course of preventative action, on a trusted professional’s word.
Find a new analogy. Now.
“But I don’t want to scare my patients.”
Patients need to be scared. Or, perhaps more realistically, and at minimum, a patient’s level of fear, or opportunity to experience fear, should be commensurate with the probability of the outcome in question.
For example, it doesn’t make sense that, currently, patients are scared of chromosomal abnormalities (before advanced maternal age), death from prematurity, SIDS, fatal injury by car accident, childhood cancer, etc., yet they’re not scared of stillbirth, even though stillbirth is statistically far more common than any of these other things.
And sometimes fear and stress, in healthy levels, inspires positive action. Like a patient who’s aware of the risk of stillbirth might monitor her baby’s movements more closely. (Though this by no means guarantees a positive outcome, I’m quite confident there are countless bereaved parents who would’ve welcomed the opportunity to find out.)
And, in what other area of medicine is this statement acceptable? Medical professionals educate on safe sleep practices. Hospital classes devote hours to car seat safety instruction. Women get mammograms to screen for breast cancer. All in attempt to avoid “scary” outcomes. Medical professionals talk about these things.
Stillbirth needs to be talked about too.
“We can’t see umbilical cords on ultrasound.”
Wrong. Google “umbilical cords on ultrasound,” and see what you find. Hint, hint – here’s what…
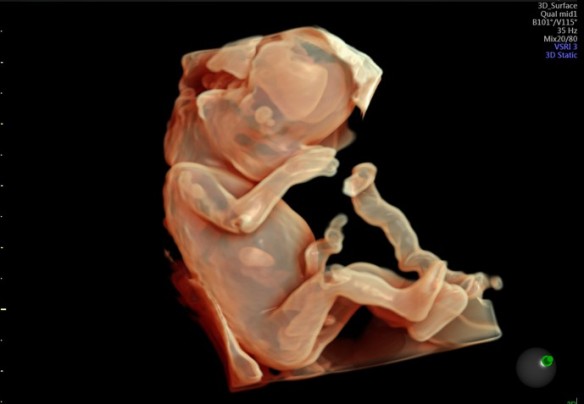

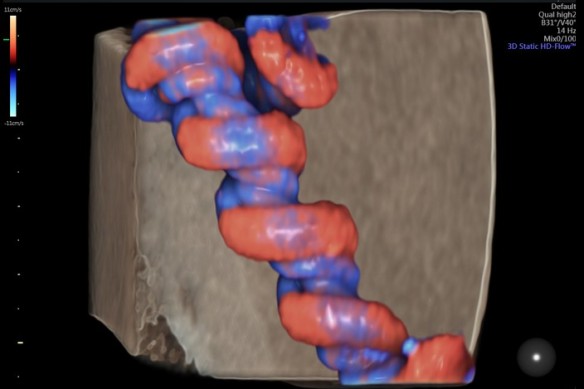
So is this a purposeful lie? Because if you admit umbilical cords can be seen on ultrasound, you might actually have to do something to attempt to prevent umbilical cord related deaths? Or are you really just so behind the times that you don’t know how to use google or your ultrasound equipment? Or have you not invested in the latest and greatest technology like GE’s apparently selling?
Whether this statement’s out of ignorance or meant to try to avoid legal liability, it needs to stop. Because it’s so obviously false to those well versed in the internet – it’s only a matter of time before patients start calling your bluff with more frequency.
And by the way, there are three key structures involved in a pregnancy – the baby, the placenta, and the umbilical cord. It’s time to start looking more closely at each of them (not just the baby). But, currently, it appears you pay little attention to the placenta and umbilical cord, and it seems as though this is to avoid legal liability too.
But in this information age, patient knowledge will catch up. And you’ll eventually be forced to pay attention, acknowledging the importance of evaluating the health of the placenta and umbilical cord within the framework of a patient’s prenatal care.
“Even if we notice umbilical cord issues, we usually don’t tell patients.”
Oh, really? Because this seems unethical. Like if you notice a patient has a deadly blood disease, do you generally tell him/her? Oh, you do? Thought so.
And I thought you couldn’t see umbilical cords on ultrasound. But now I guess you’re admitting you can. So which is it?
Patients have a right to information regarding issues they’re facing, not only so they may better understand them, but also so they may be more participative in their care as well as in important, potentially life-altering decisions, if they so desire.
“But even if we identified umbilical cord issues, what would we do about it?”
Inform the patient of the issue and the related risks. Monitor the heck out of it. Inform the patient of the increased importance of familiarizing herself with her baby’s movements. Consider early delivery. Consider C-section delivery if specific cord pathology suggests baby is at heightened risk for dying during natural labor. Give the patient options so she can actively participate in making informed decisions regarding her body and her baby, if she so chooses.
Look to the ways in which you currently monitor monoamniotic twin pregnancies, of which the greatest risk is cord entanglement.
Or simply try harder than you do now (which often seems isn’t at all).
“But so many healthy babies are born with umbilical cords wrapped around their necks.”
And 26,000 babies are stillborn each year. Approximately 8,000 of these deaths are cord-related. And do you know the difference between an innocent neck wrap and a more ominous one? Some neck wraps are more high risk for turning into deadly knots. Maybe it’s time you considered such things.
“We don’t suggest kick counts, because we’re not even sure if they matter.”
Well, maybe someone should try to determine whether they matter. Or maybe you should suggest them as part of standard practice. Just in case. Because, again, patients should know about the risk of stillbirth. And, if kick counts might matter, isn’t it better to just go ahead and perform them, erring on the side of caution?
“Make sure you count 10 kicks in a day, 10 kicks in an hour, or 10 kicks after a meal, etc.”
Ten isn’t enough. It’s best to get to know a baby’s movement patterns. If you’re going to provide instruction in this area, at least do it consistently and properly.
“Babies slow down towards the end of pregnancy. They sleep a lot.”
This isn’t true. No one, especially your affiliated medical professionals, should be perpetuating this myth. And they are. And it defies common sense. Because a full-term baby in the womb is the same baby as it is outside the womb post-delivery – a living, moving baby, who responds to stimuli and who can be awakened fairly easily. If a patient can’t get her baby to move, it’s cause for concern. And alarm. Not in three hours. Now.
“Don’t request an autopsy – most the time they won’t find anything anyway.”
While patients are certainly entitled to decline an autopsy, it should never be because one of your affiliated medical professionals is telling her “they won’t find anything anyway.” You should support full investigations into deaths of seemingly healthy babies. You should want to learn more. So you can gather the data necessary to do better.
Again, this only begins to scratch the surface with the stillbirth topic. Thus I’m confident this is only the first in a series of open notes to you.
And I’m fairly certain this isn’t a communication issue. Rather this an apathy issue and a fear of legal liability issue. You, ACOG, are a very effective communicator and disseminator of information – all your affiliated medical professionals know of your 39-week induction rule, which has been in effect for a mere few years (also a topic for another post).
All your affiliated medical professionals know the institutions with which they’re employed can win awards, some of them financial in nature, for having the highest percentage of post-39-week deliveries. (Which, on a side note, shouldn’t institutions be rewarded for the lowest percentages of deaths and life-altering medical conditions as opposed to highest percentage of post-39-week deliveries, an arbitrary benchmark that may not even appropriately apply to all patients?)
So it’s time to wake up. And get it together.
And a good start would be mandating all your affiliated medical professionals cease using these above asinine phrases – phrases that call into question your (and their) competence and insult the intelligence of all of us patients.
At the very least please give us answers that aren’t so easily disproved by google searches.
Get. It. Together.
UPDATE – I’ve emailed this note to ACOG. I’ll keep everyone posted on the response. (I hope I get a response!)

Amen! Thank you Christine for writing this open note and sharing the ultrasound pictures. Wow! I pray someone at the American Congress of Obstetricians and Gynecologists wakes up because of the content in this open letter and takes action! We can get your words out to our doctors, friends, family, co-workers, anyone, to help them see that Stillbirth prevention must be considered a priority and that the standard of care for pregnant moms must be changed. People know their own body and trust their instincts.The medical field needs to listen to the voices of their patients! These phrases MUST NOT be spoken anymore.
LikeLiked by 1 person
Thank you for your kind comment. Yes, I hope they pay attention. I plan to send this to them!
LikeLike
Incredible, Christine. I support your efforts, and I hope you won’t mind (though something tells me you won’t) if I share this across my social media networks? I so appreciate your advocacy and breadth of knowledge.
LikeLiked by 1 person
Thanks, Kim! I’ve appreciated your efforts too as it relates to Leona’s cause of death. I’d be honored if you shared – thank you!!
LikeLiked by 1 person
Thank you Christine, although I’m in the UK I’ve also had the same stupid comments about stillbirth and cord accidents. I’m so angry of the attitudes I’ve had from DRs that there is no real concern that our babies died as the majority of babies are born alive.
Max’s post mortem showed his death was caused by placenta failure (true knot as a contributory factor) he had inter uterine growth restriction- NOT PICKED up! How? My Mum was induced early 32 years ago with me as they were concerned that I was too small. Wtf? Medicine was obviously better then! My heart is broken, my life is destroyed and missing a vital piece of it forever, but I’ve been told ‘it’s sooo rare’ and ‘it’s just one of those things’ that’s ok then I’ll just carry on with my life (I can’t!) Why does it not matter that our babies have died and we can’t ever get them back? It sickens me that there are expectant parents blissfully unaware that this tragedy is on their horizon and we don’t have the power to prevent the horror that awaits them- it breaks my heart x
LikeLiked by 2 people
Ughhhh – I’m so very sorry you’re hearing these same ridiculous comments. Not only are they false, I also feel as though they minimize the value of our babies lives as well as the level of tragedy we’ve experienced.
I don’t understand why, in 2016, medical professionals continue to ignore the placenta and umbilical cord when both structures are equally vital to a baby’s health.
I too constantly think of those parents who are blissfully unaware, who will experience this tragedy tomorrow, because it happens many times each day in the United States, the UK, and throughout the world. I too am heartbroken. I’m heartbroken for me. For you. And for all of those families as well as the sweet babies robbed of their chance at life. It’s devastating and unfair. And the medical profession needs to try harder. Sending you hugs, mama. xoxo ❤
LikeLike
You’re right-It does feel like they are saying our babies ‘don’t matter’ it pisses me off and makes light of our pain. The fact that we will never be the same again.
Such simple changes can be implemented to deliver more babies alive, and ensure their parents lives aren’t destroyed forever. I will never be able to accept this was ‘meant to be’ none of our babies were meant to die! The majority were failed by our healthcare systems. We are left with that ‘feeling’ that something is missing, because there is and always will be a part of us missing 😦 x
LikeLiked by 1 person
You’re right. Lives and dreams are destroyed by this tragedy. It is very difficult to find the right words to even describe the magnitude of the effects of stillbirth – it’s enormous. And it so often seems neither society nor the medical profession understands this. I haven’t fully read the recent Lancet #EndStillbirth document, but I plan to. Apparently it addresses this – that medicine shies away from stillbirth prevention measures, in part, due to cost concerns. However, the cost of stillbirth is actually HUGE – that’s the part that it seems is being ignored, currently.
LikeLike
Yes, yes, yes. I have always said I don’t blame my OB for Lydie’s death but I do blame the protocol of care for pregnant women. I have written about many of these same issues, but not as succinctly.
Unlike most cord accidents, my Lydie had a constriction in her cord, not a nuchal cord. Would it have been visible on an ultrasound? Maybe. We’ll never know.
There’s other things I hate, like “an active baby” is a healthy baby. Lydie was my most active baby, out of 3.
I wasn’t doing kick counts, quite honestly, I didn’t know anyone who did do them at that point. Doctors seem to think Lydie’s death was “acute” and for the most part, I have chosen to believe that too. She was completely active… until she wasn’t. But I will always wish I had been paying more attention, just in case.
Thanks for writing this. I’d like to share it too if it’s okay. I freaking hate ACOG. (And also March of Dimes with the 39 week rule, but that’s another issue). Is there a way you can share it with them? I am so concerned that we are not reaching the right people.
LikeLiked by 1 person
Thank you for your comments and for your kind words. You make an excellent point with the “active baby” comment. I hate this one too. Because, as you obviously know, it’s so much more about getting to know each baby for his/her unique personality and what is normal for him/her.
I too blame standard of care, which comes back to ACOG.
I agree that some baby’s deaths are acute, and that could very well have been the case with Lydie, and we actually have reason to believe that was the case with Matthew too. But I know it isn’t always the case (with each of the 26,000/year), so I’m still very fired up about this issue. And, of course, I always think “what if?” (i.e. What if it wasn’t acute? What if we actually used technology to its full capacity? The list goes on and on and on. And I’m sick of the false claims the medical profession continues to make in regards to this topic.
Yes, please do share. Big changes are needed with ACOG. And you’re right, I didn’t even scratch the surface with the 39-week rule. (I hope to, eventually.)
I’m going to be sharing this with ACOG shortly. And I believe someone I know already did. If I get a response, I’ll update here. I’m also going to work to share it with a multitude of other parties over the next couple of days as well. And I plan to make related posts in the future too. I’m passionate about this topic, because none of the current status quo makes sense.
And I’ve been doing a bit of research to confirm who might be those best people to try to reach. I plan to possibly post some information on my blog regarding that soon, so others can know who to approach – I’m a huge believer that we patients will be a big part of initiating change through speaking out on social media.
In the meantime, thank you thank you THANK YOU for sharing. I hope they get this message. They, at minimum, need to stop spewing the type of crap I listed!
LikeLiked by 1 person
Please do keep us posted and I think you are totally right about social media. I’ve been formulating a post on generational differences regarding stillbirth and how blogs like ours are one huge difference, and hopefully something that will help to break this shit open for future generations, if not for us …
LikeLiked by 1 person
Yes, I will (just emailed ACOG). And your blog topic sounds awesome. I can’t wait to read. Keep at it, mama.
LikeLike
This is spot on. Physicians don’t measure the PLACENTA, people! When I asked Dr. Kliman why not, he said he couldn’t really answer that – he said it’s just not the paradigm or the standard of care. Doctors are taught to follow the baby and to ignore the placenta and cord. He likens this to going to the pediatrician and not having your kid weighed, and just sort of guessing about how the kid is doing. When people like him try to bring these things up to their colleagues, the doctors won’t listen (as you and others have written). The New York Times also reported recently on a paper that found doctors that overestimate fetal weight in order to pressure women in to having c-sections. Kliman thinks Luke was probably a lot smaller at his 32-week scan than we were told. So even when they’re doing the bare minimum one thing they were taught and following the baby, they’re fucking it up. Their purpose is supposed to be to bring babies safely into this world, so why do they not seem to care or want to fix the system when that doesn’t happen? I’ll never understand it. It’s like we are a whole population of people that’s just been summarily abandoned.
LikeLiked by 1 person
Couldn’t agree more. They ignore the cord and placenta. And that’s interesting what you learned about baby’s weight. (I’ll have to look for that article.) Interesting and disturbing. There are so many hidden agendas which have nothing to do with baby’s well being. Thank you for continuing to be one of the strong voices to call this out, speaking out on these important issues. I hope you continue to do so. I feel, with enough of us, we can eventually force positive change. And you sum it up perfectly with abandoned – that’s how I feel too. And it’s unacceptable. So I don’t want to quit fighting any time soon on this.
LikeLiked by 1 person
Sorry, I should have posted the link. I can’t even look at this again, it makes me so f’in angry.
http://well.blogs.nytimes.com/2016/01/11/high-birth-weight-predictions-are-often-inaccurate/?_r=0
LikeLiked by 1 person
Max was estimated at over 6 pounds at 37 weeks, but only weighed 5 pounds 15oz at birth-exactly 40 weeks. Don’t understand how they could get babies weights so wrong? My placenta was very small and this wasn’t picked up on 2 scans specifically to identify the location of the placenta. He died 12 hours before he was born because my placenta failed completely due to labour. So many missed opportunities to save our babies 😦 x
LikeLike
I’ll be sharing on Facebook. Thank you for writing this!
LikeLiked by 1 person
Great – thank you so much for sharing!
LikeLike
Such a powerful post. Thank you so much for sharing! We just got Maddy’s death certificate in the mail today (admittedly we waited a long time to submit the paperwork–too emotional). I was shocked to see the cause of her death listed as unknown. At the hospital I was told by my ob that an autopsy was not needed because it was clearly a cord accident. I asked my sister (she’s a nurse)why her certificate would be marked “unknown” if I was told it was a “fluke cord accident” and she told me that is always what is marked unless an autopsy is performed. Had I known this, I most definitely would have pushed for an autopsy. Now I’m left wondering if it was something else, and if there’s something I could have done differently. I’m angry at myself for so passively accepting the “These things just happen cord accident” speech. Definitely taking Maddy’s death certificate, and your post to my next OB appt!
LikeLiked by 1 person
Oh my gosh – that is surprising and upsetting. I’m sorry the paperwork has brought this unexpected news. I’ll be very curious as to what your OB has to say. Please keep me posted. xoxo
LikeLike
Great blog Christine! And, all soooooo accurate!
Sent via the Samsung GALAXY S®4, an AT&T 4G LTE smartphone
LikeLiked by 1 person
Thank you, Steve!
LikeLike
I love this post, Christine.
I know we’ve had many a discussion about these topics, and the stupid empty statements you describe above that make no sense.
I hate that they don’t measure the placenta. I hate that they don’t look at the cord. I hate that no one told me that the movement patterns of my baby shouldn’t change. I hate that all I did was count her kicks at random hours and that I thought that kept her safe. I hate that when her movements slowed in the days before she died I wasn’t concerned because I counted ten. I hate that I didn’t know to go in. I hate that medical professionals told me there was nothing that could be done because I don’t believe that. Not for a second.
Do you know that at one of her ultrasounds the tech actually chuckled and said, “Well she won’t be the biggest baby in the nursery.” And when I asked if she was okay I was told, “Some babies are just small.” And when I went home and looked it up ON MY OWN I first learned what the acronym IUGR stood for and no one ever mentioned it to me at any of her following appointments. Never scanned her again. Not once.
I feel responsible. I feel that I should have known something was wrong but how could I have? I was going by what they told me and what they told me wasn’t good enough. I don’t blame my doctors for following the standard of care but I blame those who maintain that it is good enough, because it is far from good enough. And now my daughter is dead and nothing will ever be good enough again.
I’m so happy you posted this, and that people are talking and sharing. We need to demand more. Lives literally depend on it.
Love you,
Nora
LikeLiked by 1 person
Thank you for your comment, Nora. Ugh, it breaks my heart – the image of you going home and finding out about IUGR on your own – them never mentioning it to you, and then losing Josie just weeks later. Pure devastation. I don’t understand why medical professional make these offhanded comments instead of perhaps investigating potential issues with the cord and placenta, things that could cause growth restriction. I too blame standard of care. It doesn’t seem it’s kept up with available technology. It will never make sense to me, which is why I intend to keep speaking out about it. Hugs to you, my friend. xoxo
LikeLike